Dr. Hu Kai: Who is at a higher risk for lymphoma? What are the symptoms? Is it curable?
Lymphoma is a common malignant tumor originating from the lymphatic hematopoietic system and is one of the cancers with a relatively high incidence rate in recent years. Although it is a malignant tumor, lymphoma is not an incurable disease. Many patients can achieve a cure and live long-term, leading normal lives just like anyone else after receiving standardized and effective treatment. In this issue, Dr. Hu Kai, Director of the Lymphoma and Myeloma Department at Beijing GoBroad Hospital, will provide a detailed and informative explanation of lymphoma to help everyone better understand and approach the disease.
1. What causes lymphoma?
Whether it is Hodgkin lymphoma or non-Hodgkin lymphoma, as a malignant tumor, the exact cause of its occurrence remains unclear. For tumors in general, they are usually caused by multiple factors. Currently, there are a few factors that may be associated with lymphoma:
First, external factors. These include exposure to radioactive materials or chemical agents. Viral infections are also a very important factor, especially certain viral infections, such as Epstein-Barr virus (EBV), hepatitis B, and hepatitis C, which have a certain relationship with specific types of lymphoma.
Second, internal factors. This mainly refers to the decline in the body's immune system, which makes it difficult to detect and eliminate the tumor in a timely manner.
When both of these factors are present, for example, an external factor like a viral infection occurs while internal immune suppression takes place for various reasons, the combined effects of these two factors can make it easier for the tumor to develop.
In fact, this mechanism is not limited to lymphoma; many other malignant tumors have a similar occurrence mechanism. Currently, it is still difficult to identify a single factor specifically responsible for the development of lymphoma.
4o mini
2. Who is at risk of developing lymphoma?
Like other malignant tumors, the specific causes of lymphoma and the high-risk groups are not yet very clear. Based on past clinical experience, immune deficiency may be a contributing factor for those more likely to develop lymphoma. For example, elderly individuals experience a decline in immune function, while children have immune systems that are not yet fully mature, which can result in a higher incidence of lymphoma in these groups. Additionally, young individuals who have immune system declines for various reasons may also be at increased risk.
From a genetic perspective, individuals with a family history of cancer are also at a higher risk of developing lymphoma or other malignant tumors.
3. What are the early clinical manifestations of malignant lymphoma?
We all want to know what symptoms might suggest a risk of lymphoma, but unfortunately, lymphoma symptoms are often very nonspecific. "Nonspecific" means that these symptoms are hard to pinpoint.
Common clinical manifestations include general symptoms such as fever, fatigue, and swollen lymph nodes, especially in areas rich in lymph nodes, such as the neck, armpits, and groin. The swollen lymph nodes are often painless and progressively enlarge.
Some lymph nodes may be located deeper in the body, so early clinical signs may be absent. When these lymph nodes become large enough to compress surrounding organs, symptoms like abdominal bloating or reduced appetite (poor appetite) may occur, especially when lymph nodes in the abdomen are enlarged.
Lymphomas may also occur in specific organs such as the spleen, which could result in spleen enlargement and discomfort, such as bloating. Other lymphomas in the central nervous system or eyes could cause neurological symptoms or affect vision.
In general, the symptoms of lymphoma are complex and nonspecific. If any discomfort arises, patients should seek medical attention promptly for appropriate diagnosis and treatment.
4. What tests are required before lymphoma treatment?
Before clinicians begin treatment for lymphoma, a detailed and comprehensive evaluation is necessary, which includes:
- First, obtaining a pathological diagnosis of lymphoma. If conditions allow, additional tests such as chromosome analysis and genetic testing may be needed to achieve an accurate diagnosis. This will be crucial for treatment planning, chemotherapy protocols, and future treatment strategies.
- Second, determining the stage of the lymphoma. Lymphoma staging differs among patients, and the treatment plan varies for early, middle, and late stages. Currently, PET-CT is the most important imaging tool used to determine the stage.
- Third, assessing the function of the patient’s organs, such as heart function, lung function, kidney function, and liver function. These evaluations help determine how much treatment intensity the patient can tolerate and provide essential information for chemotherapy dosing, regimen, and duration.
Thus, lymphoma patients need to undergo the three tests mentioned above before treatment. For patients with underlying conditions, additional tests related to these conditions may be required.
5. Is chemotherapy always necessary for lymphoma?
Although lymphoma may present with enlarged lymph nodes in local areas, it is classified as a systemic disease because the lymphatic system circulates throughout the body. For such systemic diseases, treatments like surgery or radiation therapy, which are more localized, often cannot control the disease and are generally used as auxiliary treatment methods.
Currently, chemotherapy remains the primary treatment for lymphoma. However, two important aspects must be considered:
- First, the timing of chemotherapy. Not all lymphoma patients need chemotherapy immediately upon diagnosis, especially those with indolent lymphoma without symptoms. In such cases, waiting and observation may be an option.
- Second, chemotherapy doesn't always require the use of cytotoxic drugs. Many new targeted therapies are available, and for certain types of lymphoma, chemotherapy without conventional toxic drugs may be an option. However, these cases are less common. Currently, most lymphoma patients will begin treatment with standard chemotherapy.
Thus, whether or not chemotherapy is required and when it should begin depends on the patient's clinical stage and pathological type.
6. How long can a patient live in stage III lymphoma?
Lymphoma is a systemic disease, and its symptoms are often not very prominent. As a result, many patients are diagnosed at stage III or IV. While stage III or IV lymphoma is considered to be in the middle to late stage medically, the relationship between staging and prognosis is not so clear. Many patients in these stages respond well to chemotherapy or immunotherapy and achieve complete remission, leading to long-term survival that may not be significantly different from early-stage patients.
Survival for lymphoma patients is not only related to the stage and pathological type but also to how sensitive the patient is to treatment. "Staging" only reflects the tumor load at diagnosis and its relation to prognosis, which also depends on disease type and response to treatment.
7. Can lymphoma be cured?
Whether a lymphoma patient can be cured depends on the type of lymphoma. Some types, like follicular lymphoma and chronic lymphocytic leukemia, are difficult to cure, and the goal of treatment is to extend survival and remission periods. However, high-grade lymphomas such as diffuse large B-cell lymphoma, Burkitt lymphoma, and lymphoblastic lymphoma can be cured through intensive chemotherapy.
If the tumor is cured, the short-term effects on the patient's life are typically related to treatment side effects, such as recovery of organ function, immune system function, and endocrine function. As time passes after treatment, the body gradually recovers. Long-term effects diminish as remission extends, and many cured patients can return to a healthy lifestyle, including studying and working.
Adult Lymphoma and Myeloma Department Specialties
The Adult Lymphoma and Myeloma Department primarily focuses on treating adult lymphoma and myeloma patients. Our specialty is diagnosing and treating relapsed and refractory adult lymphoma/myeloma patients.
In diagnosis, we have a specialized and precise diagnostic platform. In treatment, we offer targeted therapy, cell immunotherapy, autologous hematopoietic stem cell transplantation, allogeneic hematopoietic stem cell transplantation, and other treatment options.
Through the comprehensive application of these treatments, we aim to provide effective relief to these challenging patients, helping to extend their survival.
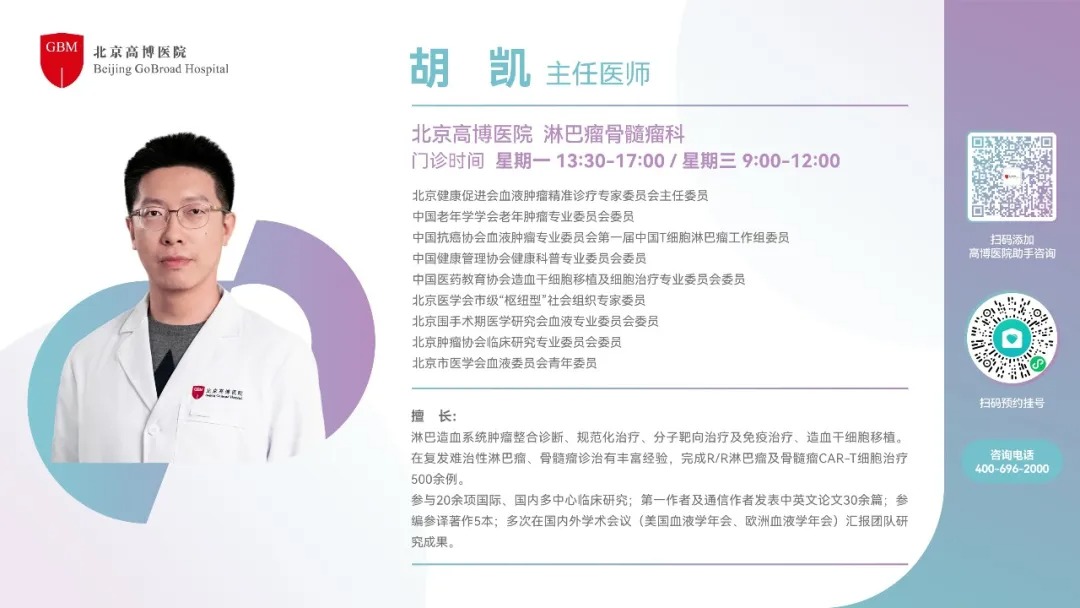
Expert Introduction