Autologous CD7 CAR-T Prepared by T Cell Depletion to Provide More Suitable Treatment for Patients with Refractory/Relapsed T-Cell Leukemia | Pan Jing Column
T-cell acute lymphoblastic leukemia (T-ALL) is a highly aggressive hematologic malignancy, and the overall prognosis for patients remains suboptimal. In recent years, given the groundbreaking advancements of chimeric antigen receptor (CAR) T-cell therapy in B-cell tumors, more and more research is focused on developing new CAR-T therapies for treating T-ALL. Donor-derived CD7-targeted CAR-T cell therapy for ALL has shown high complete remission rates, but problems such as graft-versus-host disease (GVHD) and infections have become urgent challenges that need to be addressed.
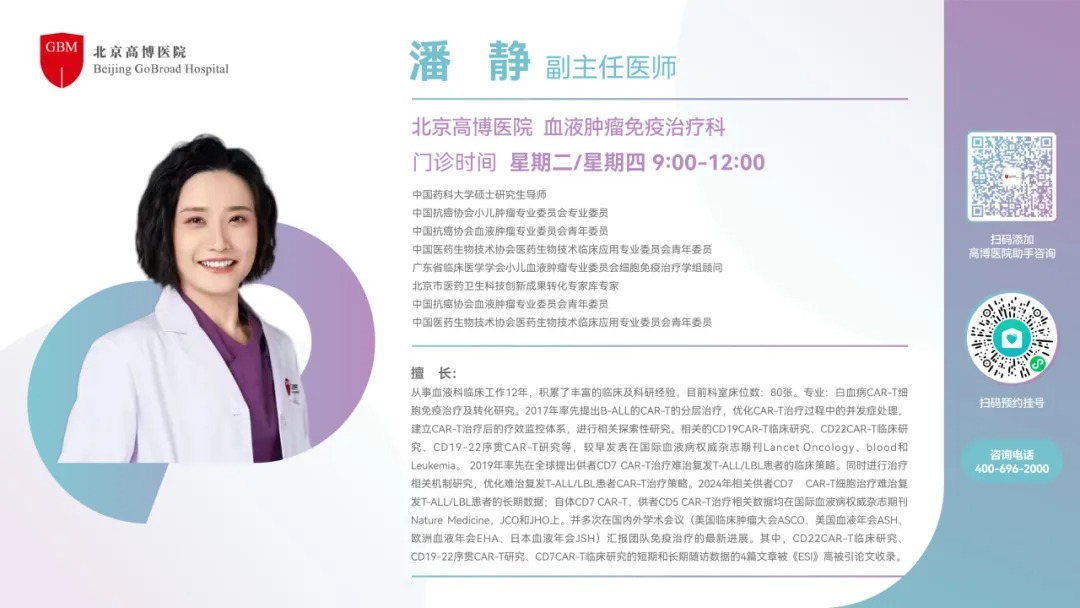
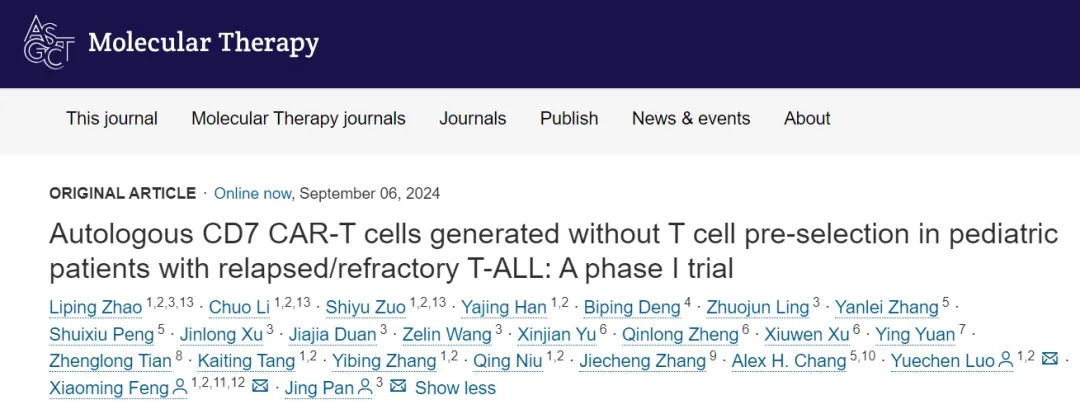
Autologous CD7 CAR-T therapy offers advantages, such as reducing the risk of GVHD, but autologous CD7 CAR-T therapies have been rare internationally so far. Recently, a study focusing on autologous CD7 CAR-T therapy for pediatric relapsed/refractory (R/R) T-ALL, titled "Autologous CD7 CAR T cells generated without T-cell pre-selection in pediatric patients with relapsed/refractory T-ALL: a phase I trial," was published in Molecular Therapy (IF: 12.4). This study preliminarily explores and reveals the preparation of autologous CD7 CAR-T cells without T-cell pre-selection, as well as its efficacy and safety in treating R/R T-ALL. The study was co-corresponded by Director Pan Jing from Beijing GoBroad Hospital of Gaobo Medical Group, Researcher Feng Xiaoming from the Chinese Academy of Medical Sciences Hematology Hospital (Institute of Hematology, Chinese Academy of Medical Sciences), and Associate Researcher Luo Yuechen.
Study Interpretation
Q1
Your team and collaborators have already conducted several studies on donor-derived CD7 CAR-T for treating r/r T-ALL and achieved high remission rates. Based on this, why did you embark on a study exploring autologous CD7 CAR-T cell preparation for r/r T-ALL patients without T-cell pre-selection?
Director Pan Jing: Since 2019, our team and collaborators began exploring CAR-T therapy for T-cell tumors, and from clinical research and practice, we gradually realized that it’s difficult to obtain sufficient normal T-cells from many T-cell tumor patients, resulting in a relatively low success rate for autologous CAR-T preparation.
At the same time, we have conducted several clinical studies on donor-derived CD7 CAR-T for treating T-cell tumors, confirming that CD7 CAR-T has a high remission rate in r/r T-ALL and r/r T-lymphoblastic leukemia/lymphoma (T-ALL/LBL). However, we also observed an increased risk of rejection and infections.
Based on this, we began to optimize the CAR-T treatment strategy, selecting more suitable CAR-T options for different T-cell tumor patients. For many T-ALL patients who have not undergone many lines of treatment, we can still collect sufficient normal and healthy lymphocytes from their bodies. We began to try preparing autologous CD7 CAR-T for them.
Additionally, regarding the preparation of T-cell CAR-T products, since the tumor cells in patients are also derived from T-cells, researchers worldwide are focusing on a key issue: how to ensure safe reinfusion of products without contamination. One possible approach to reduce CAR-T product contamination is sorting out tumor cells and normal T-cells.
However, in our early explorations, we observed that T-cell activity and quality after sorting were worse compared to unsorted T-cells. Furthermore, many patients couldn’t meet sorting criteria such as CD4 and CD8 double-negative markers, and as a result, they couldn't participate in clinical trials to benefit, which also limited the further clinical application of CAR-T.
Interestingly, we found that even without sorting, by controlling the proportion of tumor cells within a certain range, the possibility of CAR-T product contamination was very low. This is a fascinating "mathematical problem."
Therefore, we designed and conducted this phase I clinical study, which explores the key strategies for preparing autologous CD7 CAR-T without T-cell pre-selection and its efficacy and safety in r/r T-ALL. During cell culture, we performed rigorous testing, and if any positive result was detected, we would start a new round of culture to ensure the autologous CD7 CAR-T infusion was safe and uncontaminated. In fact, throughout the entire trial, we did not observe any contaminated CD7 CAR-T products, which confirmed our initial hypothesis: even without sorting, patients with tumor load in peripheral blood still have a chance for autologous CD7 CAR-T treatment. The clinical efficacy was similar to that of the donor-derived CD7 CAR-T we previously conducted, and the risk of rejection and infection after infusion was reduced. Thus, even though we have already conducted several studies on donor-derived CD7 CAR-T in T-cell tumors, we still need to find more suitable treatments for each patient, which is the key highlight of this clinical trial.
Q2
Compared to donor-derived CD7 CAR-T therapy, research on autologous CD7 CAR-T seems limited internationally. What difficulties exist in preparing autologous CD7 CAR-T for r/r T-ALL patients? Has this affected your choice of the study population in this phase I clinical trial?
Director Pan Jing: One of the challenges in this study was how to find the right patient population. Many T-ALL and T-ALL/LBL patients relapse after high-risk treatment regimens, with low lymphocyte counts, making it difficult to prepare autologous CAR-T cells.
On the other hand, regarding the potential contamination of CAR-T products by tumor cells, based on our previous research experience, we found that for patients with tumor cells in peripheral blood, the contamination rate when preparing autologous CD7 CAR-T is not as high as we initially thought. In this case, if we control the tumor load in the peripheral blood within a reasonable range, viral transfection will preferentially occur in normal T-cells, producing normal CAR-T cells that can kill surrounding tumor cells.
In this clinical trial, only a few cases of autologous CD7 CAR-T preparation were insufficient in the early stages. Later, all cases met the CAR-T product preparation standards. This confirms that removing the "sorting" step in the preparation process leads to a significant qualitative improvement in enhancing T-cell activity, increasing the final product quantity, and expanding the patient population that can benefit from it.
Q3
This study has preliminarily confirmed the feasibility of autologous CD7 CAR-T therapy without T-cell sorting in pediatric r/r T-ALL patients. How do you evaluate the preliminary efficacy and safety shown in this study?
Director Pan Jing: Overall, the preliminary results of this study demonstrate the clinical efficacy and safety we anticipated.
In the past, our several studies on donor-derived CD7 CAR-T for T-cell tumors have been presented globally, receiving significant attention and recognition from international peers. As the research progresses, we are starting to plan more suitable CAR-T treatments for different patients. The initial results of this study give us confidence that we can further clarify which patients are most suited for which CAR-T treatments. We hope that through further exploration, we can guide clinical decisions to balance optimal efficacy and safety for patients when faced with treatment choices.
Q4
Based on the current preliminary exploration results, what urgent issues do you think need to be addressed for autologous CD7 CAR-T therapy without T-cell pre-selection in r/r T-ALL patients? Do the promising results have any implications for r/r T-ALL patients who have undergone many lines of treatment or have high tumor loads?
Director Pan Jing: In fact, the concept of "not sorting" is not only a focus for our team but also for many researchers globally. I believe more teams and centers will participate in related exploration in the future.
As mentioned earlier, the current clinical challenge is that patients who have undergone multiple lines of chemotherapy have lower lymphocyte levels, making it more difficult to prepare autologous CAR-T cells even without sorting, which may lead to less ideal efficacy. Therefore, I often recommend that high-risk T-ALL and T-ALL/LBL patients freeze their peripheral blood lymphocytes within three months of diagnosis, as their physical condition and blood cells are still in relatively good condition at this time. However, it's important to note that the frozen cells are for potential autologous CAR-T treatment and do not require every patient to undergo autologous CAR-T therapy.
Q5
At the end of the article, you mentioned that phase II clinical trials are actively ongoing. Can you share the progress of this trial? What issues will you and your collaborative team focus on solving in this field moving forward?
Director Pan Jing: In phase II clinical trials, we aim to explore three main issues:
- We have conducted three cohorts to compare the efficacy and safety between autologous CD7 CAR-T, donor-derived CD7 CAR-T, and CD7 CAR-T after transplantation. Unlike our previous retrospective studies, we will summarize much more prospective data, which I believe will help address and validate many critical clinical issues.
- In 2022, the FDA launched Project Optimus, aiming to reform the dose optimization and selection model in oncology drug development. We will explore the minimum effective dose in the autologous CD7 CAR-T patient population to reduce the minimum effective dose that patients can tolerate while ensuring better clinical efficacy and safety.
- T-cell tumors with mediastinal masses have not yet achieved optimal treatment results, and we hope to explore better treatment options for these patients in the upcoming research to improve their efficacy.
Currently, our phase II clinical trial has started enrolling patients, and we have already obtained some clinical data. We hope to bring more and better treatment options to patients in our future results.
Research Summary
Autologous CD7 CAR T Cells Generated Without T-Cell Pre-Selection in Pediatric Patients with Relapsed/Refractory T-ALL: A Phase I Trial
Summary:
Chimeric Antigen Receptor (CAR) T-cell therapy has shown preliminary activity in refractory or relapsed acute T-lymphoblastic leukemia (r/r T-ALL) patients. However, clinical obstacles such as difficulties in cell preparation and infection risks remain. This phase I clinical study (NCT04840875) evaluated autologous CD7 CAR-T cells prepared without pre-selected healthy T-cells in r/r T-ALL.The study enrolled 30 patients (29 children and 1 adult), all of whom had previously received a median of 2 lines of systemic treatment and had no detectable peripheral leukemia. Except for 3 manufacturing failures, 27 (90%) patients received infusions after confirming that the product was free of leukemia contamination. Of these, 16 (59%) reached the planned target dose.
Common adverse events observed within 30 days post-infusion included: grade 3-4 neutropenia (100%), grade 1-2 cytokine release syndrome (70%), grade 3-4 (7%; including one dose-limiting toxicity), grade 1 neurotoxicity (7%), grade 2 infection (4%), and grade 2 graft-versus-host disease (4%). Two patients developed grade 2 infections after day 30.
At day 30 post-infusion, 96% of patients showed efficacy, with 85% achieving complete remission (CR) or complete remission with incomplete hematological recovery (CRi). 74% of patients underwent hematopoietic stem cell transplantation. The 12-month progression-free survival (PFS) rate was 22% (95% CI: 4-100) for transplanted patients and 57% (41-81) for non-transplanted patients.
The study shows that autologous CD7 CAR-T cells without T-cell pre-selection are feasible for treating r/r T-ALL patients.
Expert Introduction